An introduction to stroke and thrombolysis
Contents
An introduction to stroke and thrombolysis#
Stroke#
Stroke is a medical condition where blood flow to an area of the brain has been interrupted, causing cell death [1]. Stroke may be broadly categorised into two types: ischaemic, due to an arterial blockage, and haemorrhagic, due to bleeding.
Stroke is a major cause of adult long-term disability and is a major burden on healthcare services. It was estimated that in 2010, there were 5.9 million deaths and 33 million stroke survivors worldwide [2]. Eighty five thousand people are hospitalized with stroke each year in England, Wales and Northern Ireland [3]. Over the last 25 years stroke was the leading cause of lost disability-adjusted life years, which combine mortality and disability burdens [4].
Intravenous Thrombolysis (IVT)#
Intravenous thrombolysis (IVT) is a form of ‘clot-busting’ therapy developed to treat ischaemic stroke by removing or reducing the blood clot impairing blood flow in the brain.
For ischaemic strokes, IVT is an effective treatment for the management of acute stroke if given soon after stroke onset [5], and is recommended for use in many parts of the world including Europe [6]. The mechanism of action is activation of the body’s own clot-breakdown pathway, fibrinolysis. Though the benefit of alteplase is now well established, individual trials have suffered from uncertainty in the relationship between time to treatment with alteplase and the benefit achieved. Emberson et al. [5] accessed individual patient results from nine clinical trials involving 6,756 patients (3,3391 treated, 3.365 untreated control). By combining the trials in this meta-analysis, they established a statistically significant benefit of alteplase up to at 5 hours after onset of stroke symptoms, using modified Rankin Scale score of 0-1 at 3-6 months as the outcome measure. The decline in odds-ratio of an additional good outcome was consistent across age groups, but the differences in baseline (untreated) probability of a good outcome in aged under 80 and aged 80+ means that the absolute probability of a good outcome after treatment with alteplase is dependent on age group.
Figure 10 shows the probability of a good outcome if receiving alteplase, depending on time to treatment, derived from the analysis by Emberson et al.
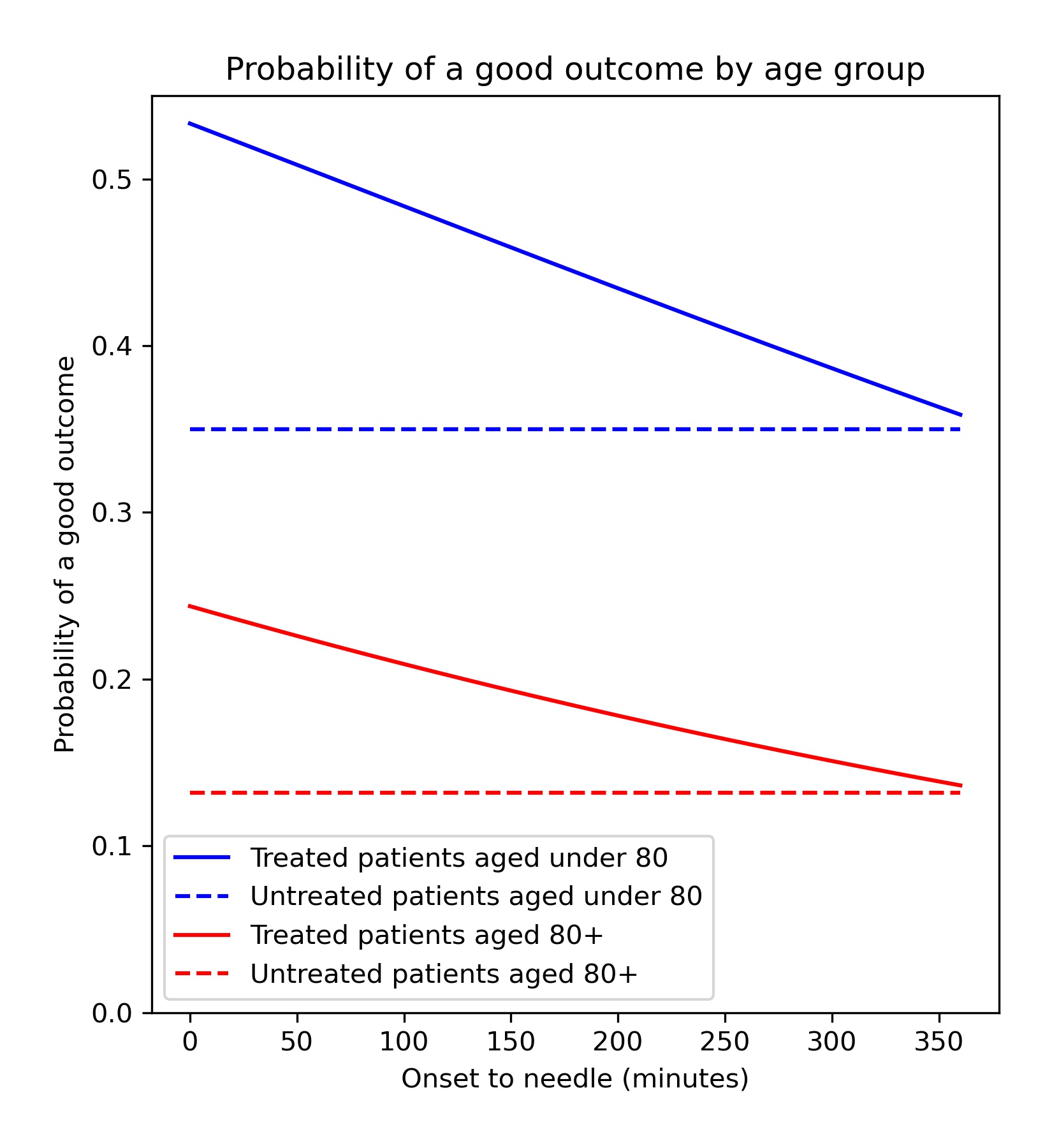
Fig. 10 Probability of a good outcome (mRS0-1) based on time from stroke onset to thtombolysis. Based om meta-analysis by Emberson et al. [5]#
Targets for IVT use and speed#
The European Stroke Organisation have prepared a European Stroke Action Plan [7], and have suggested a European target of at least 15% IVT, with median onset-to-treatment times of <120 minutes, noting that evidence suggests that achieving these targets may be aided by centralisation of stroke services [8,9]. An analysis of the IST-3 trial for thrombolysis concluded that 60% of ischaemic stroke patients arriving within 4 hours of known stroke onset were suitable for thrombolysis [10]. Assuming 40% of patients arrive within 4 hours of known stroke onset*, and 85% is stroke is ischaemic, this gives a potential target of 20% thrombolysis. The 2019/20 Sentinel Stroke National Audit Programme Report [3] provides a NHS England long term ambition of 20% emergency stroke patients receiving thrombolysis. This target to treating up to 20% of patients with thrombolysis is also stated in the NHS long term plan [11] and the specification of the Integrated Stroke Delivery Networks [12].
The NHS plan for improving stroke care through the use of Integrated Stroke Delivery Networks sets a target that patients should receive thrombolysis within 60 minutes of arrival, but ideally within 20 minutes [12]. While this speed of thrombolysis, also called door-to-needle time, provides an ambitious target, it has also been shown to be achievable as Helsinki University Central Hospital has reported median 20 minutes door-to-needle times, with 94% of patients treated within 60 minutes [13]. This speed was achieved by innovative solutions like bypassing the emergency department, and taking patients straight to the scanner (with thrombolysis delivered close to the scanner to avoid another transfer-related delay in treatment).
*In 2016-18 in England and Wales, 37% of emergency stoke patients arrived within 4 hours of known stroke onset (see results section of this report)
Barriers to thrombolysis use#
There have been many studies of barriers to the uptake of thrombolysis [14-16]. Eissa et al. [14] divided barriers into pre-admission and post-admission phases. Pre-admission barriers included poor patient response (not recognising symptoms of a stroke and not calling for help soon enough) and paramedic-related barriers (such as adding delays in getting the patient to an appropriate hospital in the fastest possible time). Hospital-based barriers include organisational problems (delay in recognising stroke patients, delays in pathway, poor infrastructure) and physician uncertainty or lack of experience leading to low use of thrombolysis. There has been significant discussion on how services may best be organised to optimise the effectiveness of thrombolysis [17].
References#
NIH National Heart Blood and Lung Institute. Stroke 2021. Available from: https://www.nhlbi.nih.gov/health-topics/stroke
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, et al. Global and regional burden of stroke during 1990-2010: Findings from the Global Burden of Disease Study 2010. Lancet 2014;383(9913):245–55. Available from: http://dx.doi.org/10.1016/S0140-6736(13)61953-4
HQIP. Sentinel Stroke National Audit Programme - Annual Report 2019-20. HQIP. 2021. Available from: https://www.hqip.org.uk/resource/sentinel-stroke-national-audit-programme-annual-report-2019-20/
Newton JN, Briggs ADM, Murray CJL, Dicker D, Foreman KJ, Wang H, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(10010):2257–74.
Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: A meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–35.
Berge E, Whiteley W, Audebert H, De Marchis GM, Fonseca AC, Padiglioni C, et al. European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur stroke J 2021 Mar 1;6(1):I–LXII. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33817340
Norrving B, Barrick J, Davalos A, Dichgans M, Cordonnier C, Guekht A, et al. Action Plan for Stroke in Europe 2018–2030. Eur Stroke J. 2018;3(4):309–36.
Bray BD, Campbell J, Cloud GC, Hoffman A, Tyrrell PJ, Wolfe CDA, et al. Bigger, faster?: Associations between hospital thrombolysis volume and speed of thrombolysis administration in acute ischemic stroke. Stroke. 2013;44(11):3129–35.
Lahr MMH, Luijckx GJ, Vroomen PCAJ, Van Der Zee DJ, Buskens E. Proportion of patients treated with thrombolysis in a centralized versus a decentralized acute stroke care setting. Stroke. 2012;43(5):1336–40.
Bembenek J, Kobayashi A, Sandercock P, Czlonkowska A. How many patients might receive thrombolytic therapy in the light of the ECASS-3 and IST-3 data? Int J Stroke. 2010;5:430–1.
NHS. The NHS Long Term Plan. 2019. Available from: https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf
NHS England and NHS Improvement. National Stroke Service Model: Integrated Stroke Delivery Networks. 2021 . Available from: https://www.england.nhs.uk/wp-content/uploads/2021/05/national-stroke-service-model-integrated-stroke-delivery-networks-may-2021.pdf
Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology. 2012;79(4):306–13. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22622858
Eissa A, Krass I, Bajorek B V. Barriers to the utilization of thrombolysis for acute ischaemic stroke. J Clin Pharm Ther 2012 Apr 13;37(4):399–409. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2710.2011.01329.x
Carter-Jones CR. Stroke thrombolysis: Barriers to implementation. Vol. 19. 2011. 53–57 p.
Engelter ST, Gostynski M, Papa S, Ajdacic-Gross V, Lyrer PA. Barriers to stroke thrombolysis in a geographically defined population. Cerebrovasc Dis. 2007;23(2–3):211–5.
Lahr MMH, Luijckx GJ, Vroomen PCAJ, Van Der Zee DJ, Buskens E. The chain of care enabling tPA treatment in acute ischemic stroke: A comprehensive review of organisational models. Vol. 260. 2013. 960–968 p.